Mediclaim (Cashless) Insurance
- Posted By Amritesh
- On April 5th, 2015
- Comments: 4 responses
Mediclaim Insurance is a Health Insurance which covers your medical and hospitalization expenses incurred by you up to the limit of sum insured. The Insurance Company reimburses the payment made by you on submission of necessary documents or directly pays to the hospital (also known as Cashless facility). These Insurance policies are offered by Public as well as Private Sectors.
The Mediclaim (Cashless) Insurance offered by non Life Insurance Companies is regulated by norms set by Insurance Regulatory Authority of India (IRDA). Insurance Companies have tie ups with certain Hospitals and Nursing Homes for providing Cashless Facility. The settlement and processing of claims is done by the TPA’s (Third Party Administrator) who are appointed by the respective Insurance providers. The TPA’s also co-ordinate with respective Hospitals to facilitate the Cashless treatment. However, it is observed that involving TPA’s often leads to delay in processing so some companies choose to settle the claims directly.
The Insurance coverage offered by most Insurers are in the range of Rs 50,000- Rs 5,00,000/-. However some Insurers are coming out with higher insurance cover, upto 1 crore. The entry age for Mediclaim Insurance is 18 years and Maximum age limit is 80 years. Companies do offer renewal up to the age of 90 years upon satisfying their terms and condition. Under Family Floater option, family members under 18 years but above 3 months can also covered under Mediclaim Benefits.
Employers also provide Mediclaim benefits to the Employees under the Group Insurance Scheme. Mediclaim Policies are also available for Retired Pensioners.
Mediclaim Insurance Premium is calculated in terms of Age of the Individual and past medical record. The premium is expectedly higher for elderly persons.
COVERAGE
The following medical expenses are covered under the Mediclaim Insurance:-
- Room, Boarding Charges.
- Nursing Care Expenses.
- Fees of surgeon, Anesthetist, physician,
- Consultants, Specialists.
- Expenses incurred on Anesthesia, blood, oxygen, operation theatre charges, surgical appliances, medicines, drugs.
- Expenses related Diagnostic materials, X-ray, Dialysis,
- Chemotherapy, Radio therapy, cost of pacemaker, Artificial limbs, cost or organs and other similar expenses.
- Certain portion of Expenses may be met by the policy in case of Ayurvedic and Homeopathy treatment depending on policy term and condition.
PRE AND POST HOSPITALIZATION EXPENSES
Expenses incurred during a certain number of days prior to hospitalization and post hospitalization expenses for a certain period from the date of discharge may be considered as part of the claim provided the expenses relate to the illness. The terms of the policy will specify it in details.
*Room Charges will be limited to a percentage of Sum Insured (Generally 1% in case of General Care and 2% in case of Intensive Care Unit (ICU).
ADDITIONAL BENEFITS
Cumulative Bonus (CB) is added to the Sum Insured in respect of each claim free period (no claims reported arising during the previous term of the policy), provided that policy is continuously renewed with any break. A certain percentage is added to the Sum Insured subject to maximum of 50% of the Sum Insured (excluding CB).
In case of a claim under the policy in respect of insured person who has earned the CB, the increased CB will by reduced by a certain percentage of the sum insured on next renewal. However, the sum insured will remain the same.
Provision for periodic Health Check up is also available as per the terms and conditions laid out in the policy by the Insurers. Normally it is available once in 4 years.
PAYMENT OF PREMIUM
Insurance in most cases needs to be renewed annually or as the terms and conditions of the policy. The premium for the policy should be paid on or before the due date. However a grace period of 15-30 days is provided after the due date for the renewal of the policy without the loss of continuity benefits. Insurance coverage is not available for the period for which no premium is received.
The premium for coverage of Rs 1,00,000/- will range between Rs 1,500- Rs 10,000/- for Individuals aged between 18-60 years. Amount of premium depends on age and various other factors.
WAITING PERIOD
Since the inception of a new policy, generally, there will be a 30 days waiting period starting from the policy inception date, during which period any hospitalization charges will not be payable by the insurance companies. However, this is not applicable to any emergency hospitalization occurring due to an accident. This waiting period will not be applicable for subsequent policies on renewal.
FREE LOOK IN PERIOD
Insured person/family is allowed a period of 15(approximately) days from the date of receipt of policy to review the terms and conditions of the policy. The policy can returned during that period and refund of the premium may be claimed.
PORTABILITY
Transfer from one Insurance Company to another is also possible, the insured person must apply with details of policy and claims to the insurer as to where and whom the policy needs to be ported.
PRE EXISTING DISEASE
Any Disease, condition, ailment, or injury or related condition for which the insured person had signs or symptoms and was diagnosed or had received medical treatment within 48 months prior to the issue of first policy by the company will be excluded from Insurance coverage.
However, on Insurance continued beyond 48 months, the pre existing disease, condition, ailment or injury will be covered under the Policy.
EXCLUSIONS
The following are generally excluded under health policies:
- All pre-existing diseases (the pre-existing disease exclusion is uniformly defined by all non life and health insurance companies).
- Under first year policy, any claim during the first 30 days from date of cover, for sickness / disease. This is not applicable for accidental injury claims.
- During 1stand 2nd year of cover – cataract, Benign prostatic hypertrophy, Hysterectomy for Menorrhagia or Fibromyoma, Hernia, Hydrocele, Congenital Internal diseases, Fistula in anus, piles, sinusitis and related disorders.
- Circumcision unless for treatment of a disease.
- Cost of spectacles, contact lenses, hearing aids.
- Dental treatment / surgery unless requiring hospitalization.
- Convalescence, general debility, congenital external defects, V.D., intentional self-injury, use of intoxicating drugs / alcohol, AIDS, Expenses for Diagnosis, X-ray or lab tests not consistent with the disease requiring hospitalization.
- Treatment relating to pregnancy or child birth including cesarean section.
- The actual exclusions may vary from product to product and company to company. In group policies, it may possible to waive / delete the exclusions on payment of extra premium.
*Some of the Insurance companies are offering Maternity Cover, but it comes with a long waiting period and additional premium.
PREFERRED PROVIDER NETWORK (PPN)
It is a network of hospitals which have agreed to provide cashless treatment to the insured person. The list is provided by the company to the insured person at the time of purchasing the policy.
CLAIM PROCEDURE
In case of claim, the insured person/family’s representative/agent shall intimate the TPA/Company through letter, e-mail, fax providing all relevant information relating to claim including plan of treatment, policy number within prescribed time limit.
FOR CASHLESS CLAIMS
- In case of Planned Hospitalization: At least 72 hours prior to insured person’s admission to Network Provider/PPN.
- In case of Emergency Hospitalization: Within 24 hours of the insured person’s admission to network provider/PPN.
- Treatment should be taken in a network provider/PPN pre authorized by TPA/Company.
- Application in proper form from network provider/PPN and should be sent to TPA/Company.
- TPA/Company to verify claims before processing it.
FOR REIMBURSEMENT CLAIMS
- In case of Planned Hospitalization: At least 72 hours prior to insured person’s admission to Network Provider/PPN.
- In case of Emergency Hospitalization: Within 72 hours of the insured person’s admission to network provider/PPN.
- Documents related to treatment and expenses should be submitted to the TPA/Company.
- All Cash Documents in Original needs to be submitted.
- Submission of documents to be completed within the time limit of 15 days of discharge or as mentioned in the policy.
(It may vary for some policies.)
SETTLEMENT OF CLAIMS
On receiving the final documents or report, the claim shall be settled within a period of 30 days. If company fails to do so, it has to pay interest above the prevalent bank rate on the outstanding amount till it is cleared.
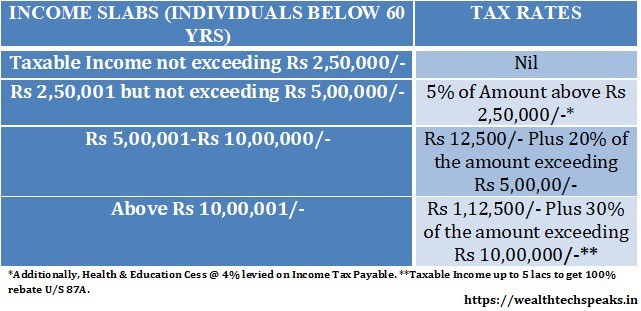
TAX BENEFITS
Tax Deduction is available on the premium pay for Health Insurance U/S 80D up to Rs 25,000/- for Individuals. Senior Citizen can avail deductions up to Rs 30,000/- on the premium paid.
COMPANIES PROVIDING MEDICLAIM INSURANCE
Some of the private and public sector companies providing Mediclaim Insurance is provided below:-
New India Assurance (Public)
National Insurance (Public)
Max Bupa (Private)
Bharati Axa (Private)
*There are many other companies too providing the same.
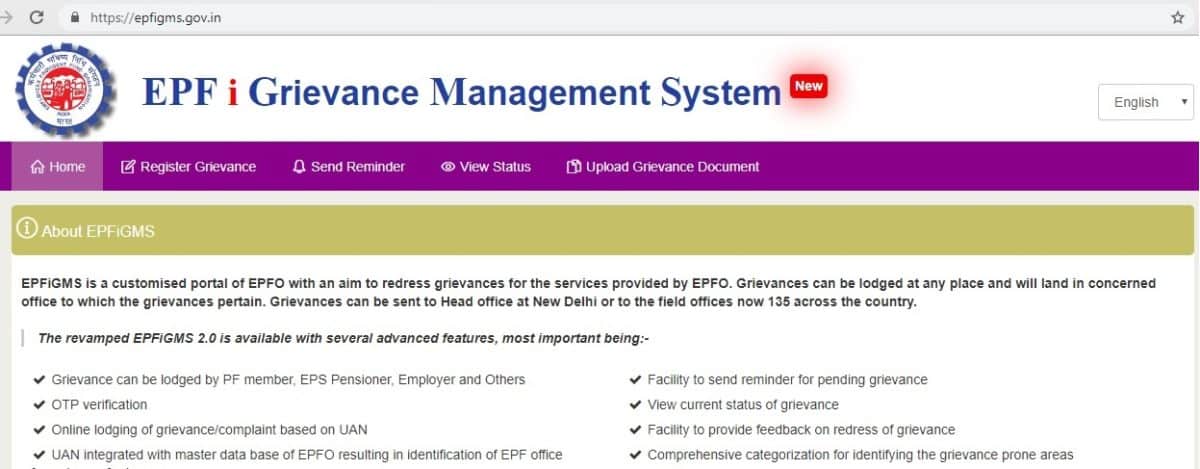
GRIEVANCE REDRESSAL
If you have any grievance against the Insurer or any policy you can get in touch with the IRDAI on the Toll Free Number 155255 or you can also email them at complaints@irda.gov.in
Read more about Health Insurance and Critical Ilness Insurance in the link given below:-
Accident Insurance Policy
Critical Illness Insurance
Health Insurance: Need for Health Insurance
Read more about Health Insurance and Critical Ilness Insurance in the link given below:-
Accident Insurance Policy
Critical Illness Insurance
Health Insurance: Need for Health Insurance
www.amritfinaa.blogspot.com



Your style is so unique compared to other folks I have read stuff from. Thank you for posting when you have the opportunity, Guess I will just bookmark this blog.
Very good info. Lucky me I came across your site by chance (stumbleupon). I’ve bookmarked it for later.
The very next time I read a blog, Hopefully it does not fail me just as much as this one. I mean, I know it was my choice to read, but I truly believed you would probably have something useful to talk about. All I hear is a bunch of whining about something that you could possibly fix if you were not too busy seeking attention.
You ought to be a part of a contest for one of the best websites on the web. I’m going to recommend this site!